The 3 Masters Series 2026

Kuala Lumpur Convention Centre, Kuala Lumpur, Malaysia
Presenters
📅 Save the Date: 5–8 February 2026
📍 Kuala Lumpur Convention Centre, Malaysia
The 3 Masters Series returns in 2026, bigger, bolder, and more unified than ever! This 2026, we unite world-renowned masters in prosthodontics, implantology, aesthetic dentistry, digital dentistry, orthodontics, paediatric & myofunctional dentistry and more.
What to expect:
- 1 Bonus Day Lecture
- 3 Full Day of Deep Learning
- 12 Hands-On Workshops across multiple disciplines
- Exhibitions by Sponsors
- Case Discussion Forums
- Scientific Poster Competition
💥 Exclusive Workshop Rebates
- Buy 2 workshops → SGD 300 rebate
- Buy 3 workshops → SGD 450 rebate
- Buy 4 workshops → your 3 Masters Series ticket is waived
Whether you’re a general dentist, digital workflow enthusiast, implant expert or specialists, this is the place to be. Register now!
Workshop Schedule
6th Feb 2026
08:00-11:00: Prof. Irena Sailer 11:00-14:00: Dr. Kris Chmielewski 15:00-18:00: Dr. Stanley Liu7th Feb 2026
09:00-12:00: Prof. Markus Hürzeler 11:00-14:00: Dr. Sepehr Zarrine 15:00-18:00: Dr. Irene Lau8th Feb 2026
08:00-11:00: Prof. Hom Lay Wang 12:00-15:00: Prof. James Chow 12:00-15:00: Dr. Donny Mandrawa 15:00-18:00: MDT Edris Rasta9th Feb 2026
09:00-17:00: Dr. Marko Jakovac 09:00-12:00: Dr. Stephanie YeungAvailable Workshops

Defect-oriented rehabilitation in tooth wear: strategic vertical dimension reestablishment for long-term success
Prof. Dr. Irena Sailer & MDT Vincent Fehmer
February 6, 2026 | 08:00 - 11:00 | Ancora Imparo Event HallKey topics: Tooth Wear Management, Vertical Dimension, Defect Analysis
S$1200

Prosthetically guided free-hand immediate implantation and loading with prefabricated crown shell
Dr. Kris Chmielewski
February 6, 2026 | 11:00 - 14:00 | M.Vision CenterKey topics: Immediate Implant Placement, Crown Shell Technique, Guided Bone Regeneration
S$600
Sleep apnea - Diagnosis and dental management
Dr. Stanley Liu
February 6, 2026 | 15:00 - 18:00 | AI Event HallKey topics: Sleep-disordered breathing diagnosis, Oral appliance therapy, Airway assessment
S$800
Advanced oral soft tissue reconstruction
Prof. Markus B. Hürzeler
February 7, 2026 | 09:00 - 12:00 | M.Vision CenterKey topics: Soft tissue requirements around implants, Surgical techniques, Aesthetic zone management
S$1500

Zygomatic Implants essentials: indications, techniques & Hands-On discovery
Dr. Sepehr Zarrine
February 7, 2026 | 11:00 - 14:00 | M.Vision CenterKey topics: Zygomatic Implants, Surgical Techniques, Case Selection
S$800

Why tongue tie affects growth and airway?
Dr. Irene Lau
February 7, 2026 | 15:00 - 18:00 | M VisionKey topics: Ankyloglossia diagnosis, Treatment planning, Surgical techniques
S$600

Advanced flap designs for soft and hard tissue augmentation. Keys for long-term implant stability
Prof. Hom Lay Wang
February 8, 2026 | 08:00 - 11:00 | M.Vision CenterKey topics: Hard tissue regeneration, Soft tissue management, Biomaterial selection
S$1350
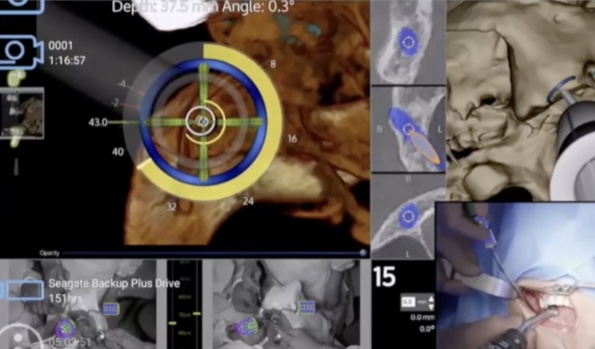
AI-Integrated Full Arch Protocol: Advancements in Navigation, Imaging, Robotic Surgery, and Manufacturing
Prof. James Chow
February 8, 2026 | 11:00 - 14:00 | AI Event HallKey topics: Augmented reality applications, Emerging technologies, Digital restoration design
S$600

Biomimetic microstaining technique
MDT Edris Rasta
February 8, 2026 | 15:00 - 18:00 | M VisionKey topics: Camera settings, Lighting techniques, Clinical photography protocols
S$800

Digital protocol in aesthetic dentistry and micro-preparation (hands-on on phantom heads)
Dr. Marko Jakovac
February 9, 2026 | 09:00 - 17:00 (Full Day) | M.Vision CenterKey topics: Digital integration in esthetic treatment, Micro-preparation techniques, Conservative esthetics
S$1800

Leveraging 3D printing for provisionalization: from removable to fixed prostheses
Dr. Stephanie Yeung
February 9, 2026 | 09:00 - 12:00 | KLCC Event CenterKey topics: 3D printing technologies, Removable prosthesis workflows, Fixed prosthesis workflows
S$600

Myofunctional Dentistry 101: What Every Dentist Should Know
Dr. Donny Mandrawa
February 8, 2026 | 12:00 - 15:00 | KLCC Event CenterKey topics: Muscle function and jaw growth, Sleep quality, Red flags in assessment
S$600
Explore Malaysia! Take advantage of these curated tour packages during your stay.

Kuala Lumpur by Day
Discover iconic landmarks: Batu Caves, National Mosque, Independence Square, and KL Tower.
Half Day Tour
Kuala Lumpur Night Vibes
Experience KL at night: Petronas Towers views, Jalan Alor food street, and vibrant nightlife.
Evening Tour
Melaka Day Trip
UNESCO Heritage City: Dutch Square, A Famosa Fort, Jonker Street, and river cruise.
Full Day Tour
Tea Fields & Old City Vibes
Cameron Highlands & Ipoh: BOH Tea Plantation, strawberry farms, and heritage old town.
Full Day Tour
Tea Fields & Cave Visiting
Nature adventure: Cameron Highlands tea plantations and Gua Tempurung cave exploration.
Full Day Tour
Tropical Forest Explorer
Taman Negara rainforest: Canopy walkway, jungle trekking, and wildlife spotting adventure.
2-Day AdventureThe 3 Masters 2026 - A Four-Day Journey to the Future of Dentistry
Thursday, 5th February - Conference Day
| 07:30 | Registration open |
| 09:00 | Opening words |
| 09:20 | Dr. Stanley Liu - Designing smiles that sleep and breathe |
| 10:10 | Dr. Donny Mandrawa - Rewriting Dentistry: Why Myofunctional Dentistry is the Future |
| 11:00 | Dr. Sepehr Zarrine - Zygomatic Implants: Streamlined protocols and precision |
| 11:50 | Coffee break |
| 12:10 | Dr. Kris & Dr. Maja Chmielewski - Digital implantology in practice |
| 13:00 | Lunch break |
| 14:00 | Dr. Nuno Sousa Dias - Teeth alignment as a mandatory step in complex treatment planning |
| 14:50 | Dr. Irena Sailer & MDT Vincent Fehmer - Precision by design: digital pathways to predictable implant-supported restorations |
| 15:40 | MDT Edris Rasta - Practical guidance on integrating digital tools into daily clinical practice |
| 16:30 | Coffee break |
| 16:50 | Dr. Jeanette Chua - Can we still practice solo? |
| 17:40 | All Speakers - Forum & Q&A |
Friday, 6th February - Master Craig Misch
| 08:30 | Welcoming guests |
| 09:05 | Craig Misch - Current trends in bone augmentation - Part 1 |
| 11:00 | Coffee break |
| 11:20 | Craig Misch - Current trends in bone augmentation - Part 2 |
| 13:00 | Lunch break |
| 14:00 | Craig Misch - Current trends in bone augmentation - Part 3 |
| 15:30 | Coffee break |
| 16:05 | Craig Misch - Current trends in bone augmentation - Part 4 |
Saturday, 7th February - Master Marko Jakovac
| 08:30 | Welcoming guests |
| 09:05 | Marko Jakovac - Protocol in oral rehabilitation: from analog to digital - Part 1 |
| 11:00 | Coffee break |
| 11:20 | Marko Jakovac - Protocol in oral rehabilitation: from analog to digital - Part 2 |
| 13:00 | Lunch break |
| 14:00 | Marko Jakovac - Protocol in oral rehabilitation: from analog to digital - Part 3 |
| 15:30 | Coffee break |
| 16:05 | Marko Jakovac - Protocol in oral rehabilitation: from analog to digital - Part 4 |
Sunday, 8th February - Master Markus Hürzeler
| 08:30 | Welcoming guests |
| 09:00 | Prof. Markus Hürzeler - With the future in view - clinical decision making in the course of patients' lives |
| 10:00 | Prof. Markus Hürzeler - New ideas about soft tissue management in plastic reconstructive surgery |
| 11:00 | Coffee break |
| 11:30 | Prof. Markus Hürzeler - The socket-shield technique: new trends and new insights |
| 13:00 | Lunch break |
| 14:00 | Prof. Markus Hürzeler - Simplifying implant therapy in the sense of the patient expectations |
| 15:30 | Coffee break & Closing |
5th Feb Ancora Imparo 10th Year Anniversary
1. Dr. Nuno Sousa Dias - Teeth alignment as a mandatory step in complex treatment planning
2. Dr. Kris Chmielewski & Dr. Maja Chmielewska - Digital Implantology in Practice: Guided Surgery Workflows in the Esthetic Zone and Full Arch Rehabilitation
3. Dr. Stanley Liu - Designing Smiles that Sleep and Breathe
4. Dr. Sepehr Zarrine Zygomatic Implants: Streamlined protocols and precision as game-changers for severe atrophies
5. Dr. Jeanette Chua - Can we still practice solo?
6. MDT Edris Rasta - Receive practical guidance on integrating digital tools into daily clinical practice
7. Prof. Irena Sailer & MDT Vincent Fehmer - Precision by Design: Digital Pathways to Predictable Implant-Supported Restorations
8. Dr Dr Henry He Gang - Dynamic Navigation, The Next Level…
9. Dr Donny Mandrawa - Rewriting Dentistry: Why Myofunctional Dentistry is the Future
10. Dr Irene Lau - Foundations for the Future: Childhood Airway and Growth Influencing Adult Outcomes
6th Feb Dr. Craig Misch: Current trends in Bone Augmentation
- To understand the factors that determine the selection of a bone augmentation technique and materials.
- To understand when autogenous bone is needed for specific cases of bone augmentation.
- To understand how bone volume gains influence the decision to use particular techniques and materials for bone augmentation.
- To understand when narrow diameter implants or short implants may be an alternative to bone augmentation.
7th Feb Prof Marko Jakovac: Protocol in Oral Rehabilitation: from Analog to Digital.
- Understand the principles of oral rehabilitation
– Define the key components of full-mouth rehabilitation and identify common clinical indications. - Evaluate digital protocols in prosthetic dentistry
– Compare traditional analog vs. digital approaches in treatment planning, design, and execution. - Integrate digital technology into clinical protocols
– Understand the process from digital impression to final prosthetic fabrication, including material selection and lab communication. - Plan and execute full-mouth rehabilitations using a digital protocol
– Develop a step-by-step workflow for complex cases, including esthetic and functional considerations. - Recognize potential complications and troubleshooting strategies
– Identify common challenges in digital rehabilitation cases and learn how to prevent or resolve them. - Collaborate effectively with the digital dental team
– Optimize communication between clinician, technician, and patient throughout the digital workflow.
8th Feb Prof. Dr. Markus Hurzeler: New Trends in Implant Dentistry
Implant therapy has undergone tremendous changes over the past decade. Ten years ago, it became increasingly clear that dental implants could create several challenges. The development of mucositis and peri-implantitis has gained more attention. Preventing these diseases is now a major focus. Today, we have a greater understanding of what must be done to establish stable clinical outcomes around dental implants. Additionally, immediate implant placement—which is characterized by shorter treatment times, reduced effort, and fewer surgical interventions has received increasing attention. While survival rates of immediately placed implants appear similar to those of delayed or late implant placements, aesthetic failures, such as mid-facial and interproximal soft tissue volume loss, remain common challenges. To address soft tissue deficiencies inpost-extraction sites, various clinical recommendations and a lveolar ridge preservation techniques have been described in the literature. These methods have shown a significant reduction invertical and horizontal defect formation following tooth extraction, compared to unassisted socket healing. However, systematic literature reviews consistently conclude that while post-extraction resorption of the a lveolar ridge can be limited, it cannot be entirely avoided. If the goal is to enable more implant patients to benefit from immediate implant placement in the future, preventing the loss of periodontal ligament and bundle bone after tooth removal is essential. Furthermore, it is crucial to pay close attention to the patients' wishes and expectations during implant therapy.
- Understand new aspects of maintaining teeth orplacing implants.
- Learn about new ideas for soft tissue management around implants andteeth.
- Gain insights into the socket-shield technique.
- Understand the new trends in implantdentistry.
View Workshops title here!
1. Prof. Irena Sailer & MDT Vincent Fehmer - Defect-Oriented Rehabilitation in Tooth Wear: Strategic Vertical Dimension Reestablishment for Long-Term Success
2. Prof. Markus Hürzeler - Advanced oral soft tissue reconstruction
3. Prof. Marko Jakovac - Digital Protocol in Aesthetic Dentistry and Micro-Preparation (Hands-on on phantom heads)
4. Dr. Kris Chmielewski - Prosthetically guided free-hand immediate implantation and loading with prefabricated crown shell in esthetic region and guided bone regeneration
5. Dr. Sepehr Zarrine - Zygomatic Implants essentials: indications, techniques & Hands-On discovery
6. Prof. Hom-Lay Wang - Advances flap designs for soft and hard tissue augmentation and keys for long-term implant stability
7. Prof. James Chow - AI-Integrated Full Arch Protocol: Advancements in Navigation, Imaging, Robotic Surgery, and Manufacturing Techniques
8. Dr. Stanley Liu - What Dentists Should Know About Sleep-Disordered Breathing: From Diagnosis to Intervention
9. Dr. Irene Lau - why tongue tie and lip ties affects airway and craniofacial development
10. MDT Edris Rasta - Biomimetic microstaining technique
11. Dr Donny Mandrawa - Myofunctional Dentistry 101: What Every Dentist Should Know
12. Dr Stephanie Yeung - Leveraging 3D printing for provisionalization: from removable to fixed prostheses
























