THE 3 MASTERS

Implementing A Risk Assessment Strategy In Clinical Practice: Emphasis on Occlusion - Dr. John Kois
The fundamental rationale for a comprehensive treatment approach is a long-term strategy for dental health commensurate with an enhanced level of wellness for our patients. Understanding parameters of disease expression is sometimes confused because of misguided science or parameters that have led to patient adaptation. Formulating specific treatment needs based on an individual’s risk assessment has created new challenges for both the dentist and the patient. Until we have more objective data with better metrics, much of our clinical decision making will remain emotionally driven and empirical.
For example, our knowledge about occlusion has been based on gnathologic principles. These concepts are the basis of a mechanical system with focus on posterior determinants and mutual protection. If it is that simple, why can’t we predict when or why occlusal pathology develops or why can’t we always create a therapeutic occlusion? This program will focus on biologic principles necessary for developing a functional occlusion. New paradigms will be presented to enlighten participants about understanding occlusal problems.
Learning objectives:
A systematic approach for treatment planning every patient in their practice.
To focus on the four most important diagnostic categories.
Understanding the difference between occlusal disease and functional adaptation.
To develop critical risk parameters to minimize failures and maximize successful results.
Protocols to implement treatment planning strategies.
New Perspectives on Vertical and Horizontal Augmentation - Dr. Istvan Urban
Vertical and horizontal augmentation presents one of the greatest challenges of bone regeneration in implant dentistry. This is primarily due to the difficulty of the surgical procedure and its potential complications. Patient selection, patient preparation for surgery, precise surgical techniques and postoperative management are the key factors in reducing the rate of bone graft complications.
To predictably achieve successful bone augmentation angiogenesis, clot stability and space maintenance should be employed.
Another important factor is flap closure during bone augmentation. The key to achieving wound closure is not only the clinician’s ability in obtaining tension free release flap but also good soft tissue quality and quantity. In an attempt to achieve wound closure and hence graft stability, the buccal mucosa are often broadly released, and this often results in a severe apical translocation of the mucogingival line, loss of vestibule and keratinized mucosa (KM).
Recent research on vertical and horizontal ridge augmentation as well as soft tissue reconstruction will be presented.
Utilizing these procedures may lessen the need of harvested autogenous bone and may generally lead to decreased morbidity and therefore increased patient comfort and satisfaction associated with these regenerative procedures.
Learning objectives:
- Understand the biology of the incorporation of the bone graft.
- Understand the surgical anatomy of the floor of the mouth
- Learn the surgical principles of ridge augmentation surgery
- Learn the surgical principles of the reconstruction of the vestibule and keratinized tissue after ridge augmentation.
Optimizing Peri-Implant Esthetics: Ortho-Perio-Restorative Connection - Dr. Joseph Kan
Achieving anterior implant esthetics is a challenging and demanding procedure. To create implant restorations with harmonious gingival contour that emulate nature is a fusion of science and art. Understanding the biologic and physiologic limitations of the soft and hard tissue will facilitate predictability in simple to complex esthetic situations.
This presentation encompasses the Science, Art and Limitations of Orthodontics, Periodontics and Restorative Dentistry on esthetic implant reconstruction. Current implant treatment philosophies and methodologies for replacing currently missing teeth and the management of patients who will be losing a tooth or teeth in the esthetic zone will be discussed. Emphasis will be placed on diagnosis and treatment planning, surgical and prosthetic management of soft and hard tissue for optimal anterior implant esthetics.
Leaning Objectives
- Interdisciplinary Diagnosis & Treatment from single to multiple teeth replacement in the esthetic zone.
- Identify prognostic variables for predictable implant esthetics
- Implant papilla management
- Immediate tooth replacement: IS it a viable procedure?
- Myth & reality of prosthetic emergency profile
- Current concepts on flap & incision designs
- Bone and gingival grafts: What is possible, what is not possible?
- Orthodontics site development: What we know, what we do not know?
- Complications management
Do you want to apply any available grant for this course?
Workshop Details

Defect-oriented rehabilitation in tooth wear
Strategic Vertical Dimension Reestablishment for Long-term Success
Prof. Dr. Irena Sailer & MDT Vincent Fehmer
Date
Feb 6, 2026
Time
08:00 - 11:00
Level
Advanced
Fee
S$1,200
Workshop Overview
This workshop presents a structured, defect-oriented approach to managing patients with severe tooth wear—focusing on preserving tooth structure, restoring function, and achieving long-term esthetic and biological success.
Diagnostic Protocols
Evaluating VDO in wear patients using diagnostic wax-ups and mock-ups
Restorative Planning
Adhesive techniques in minimally invasive full-mouth reconstructions
Digital Workflow
Integrating digital tools in diagnostics, design, and fabrication
Learning Objectives
- Master defect-oriented analysis techniques for worn dentitions
- Apply adhesive techniques in minimally invasive reconstructions
- Select appropriate materials based on wear patterns
- Integrate digital tools in diagnostics and fabrication
- Coordinate interdisciplinary care for predictable outcomes

Prof. Dr. Irena Sailer
Professor of Fixed Prosthodontics

MDT Vincent Fehmer
Master Dental Technician
About the Instructors
Prof. Dr. Irena Sailer is Chair of Fixed Prosthodontics and Biomaterials at the University of Geneva, Switzerland. She is internationally recognized for her research on digital workflows, ceramic materials, and tooth wear rehabilitation protocols.
MDT Vincent Fehmer is a Master Dental Technician working closely with Prof. Sailer. He is known for his expertise in digital dental technology, CAD/CAM fabrication, and achieving excellence in aesthetic restorations through innovative laboratory techniques.
Areas of Expertise
- Fixed Prosthodontics
- Tooth Wear Management
- Digital Workflows
- Ceramic Materials
- CAD/CAM Fabrication
- Adhesive Dentistry
Who Should Attend
- Prosthodontists managing complex wear cases
- Restorative dentists seeking advanced techniques
- General dentists interested in full-mouth rehabilitation
- Dental technicians working with digital workflows
- Practitioners treating bruxism and erosion patients
Workshop Features
- Evidence-based diagnostic protocols
- Digital workflow demonstrations
- Interdisciplinary case discussions
- Digital protocols manual
- Certificate of completion
Workshop Details

Prosthetically guided free-hand immediate implantation and loading
Prefabricated Crown Shell in Esthetic Region & Guided Bone Regeneration
Dr. Kris Chmielewski
Date
Feb 6, 2026
Time
11:00 - 14:00
Level
Advanced
Fee
S$600
Workshop Overview
This workshop provides comprehensive training in prosthetically guided immediate implant placement with prefabricated crown shells in the esthetic region, combined with guided bone regeneration techniques for optimal hard-tissue support.
Pre-surgical Planning
Implant positioning guided by prosthetic outcome for optimal esthetic results in the anterior zone.
Freehand Technique
Atraumatic extraction and implant placement without surgical guides for experienced clinicians.
GBR Techniques
Guided bone regeneration protocols for optimal hard-tissue support around immediately placed implants.
Learning Objectives
- Master prosthetically guided immediate implant placement techniques
- Learn atraumatic extraction and freehand implant placement protocols
- Implement immediate provisionalization with prefabricated crown shells
- Apply guided bone regeneration for optimal hard-tissue support

Dr. Kris Chmielewski
Implant Surgery & Immediate Loading Specialist
Dr. Kris Chmielewski is a renowned expert in immediate implant placement and loading protocols, with extensive experience in esthetic zone rehabilitation and guided bone regeneration techniques.
Areas of Expertise:
- Immediate implant placement in extraction sockets
- Freehand surgical techniques
- Crown shell provisionalization
- Guided bone regeneration protocols
Who Should Attend
- Implant surgeons interested in immediate placement techniques
- Prosthodontists seeking to expand their surgical skills
- General dentists performing implant surgery
- Clinicians focused on esthetic zone rehabilitation
- Practitioners interested in minimally invasive techniques
Workshop Features
- Pre-surgical planning protocols
- Freehand implant placement demonstration
- Crown shell provisionalization techniques
- GBR implementation guidelines
- Certificate of completion
Workshop Details
What dentists should know about sleep-disordered breathing
From Diagnosis to Intervention
Dr. Stanley Liu
Date
Feb 6, 2026
Time
15:00 - 18:00
Level
Intermediate
Fee
S$800
Workshop Overview
This comprehensive workshop provides dentists with essential knowledge and practical skills to identify, screen, and manage patients with sleep-disordered breathing. Learn to integrate sleep medicine principles into your dental practice through evidence-based protocols.
Sleep-Disordered Breathing
Comprehensive understanding of sleep apnea pathophysiology and its systemic effects on patient health.
Screening & Diagnosis
Learn validated screening protocols and diagnostic criteria for identifying sleep-disordered breathing in dental patients.
Oral Appliance Therapy
Master the selection, fitting, and management of mandibular advancement devices for sleep apnea treatment.
Learning Objectives
- Recognize signs and symptoms of sleep-disordered breathing during routine dental examinations
- Implement evidence-based screening protocols in your dental practice
- Understand indications and contraindications for oral appliance therapy
- Collaborate effectively with sleep physicians and other healthcare providers
Dr. Stanley Liu
Sleep Medicine & Dental Sleep Medicine Specialist
Dr. Stanley Liu is a leading expert in the field of dental sleep medicine, with extensive experience in diagnosing and treating sleep-disordered breathing conditions. He has trained numerous dental professionals in implementing sleep medicine protocols in their practices.
Areas of Expertise:
- Sleep-disordered breathing diagnosis
- Mandibular advancement device therapy
- Multidisciplinary sleep care coordination
- Practice integration of sleep medicine
Who Should Attend
- General dentists interested in sleep medicine integration
- Practitioners treating patients with snoring complaints
- Dentists wanting to offer oral appliance therapy
- Clinicians interested in multidisciplinary patient care
- Dental professionals seeking to expand services
Workshop Features
- Sleep-disordered breathing screening protocols
- Diagnostic criteria and assessment tools
- Oral appliance therapy guidelines
- Interdisciplinary collaboration frameworks
- Certificate of completion
Workshop Details
Advanced oral soft tissue reconstruction
Optimizing Soft Tissue Outcomes Around Implants
Prof. Markus B. Hürzeler
Date
Feb 7, 2026
Time
08:00 - 11:00
Level
Advanced
Fee
S$1,500
Workshop Overview
Soft tissue management has become a cornerstone of successful implant therapy. As understanding of peri-implant biology grows, so does the need for tailored surgical approaches that differ from those used around natural teeth.
In this workshop, Prof. Markus Hürzeler will present advanced concepts and clinical techniques to optimize soft tissue outcomes around implants, with a focus on both function and aesthetics.
Soft Tissue Requirements
Critical role of soft tissue thickness in maintaining peri-implant bone. Understanding why traditional periodontal techniques cannot be directly applied to implants.
Surgical Techniques
Modified free gingival grafts for implant sites. Use and limitations of apically repositioned flaps. Optimal donor sites for connective tissue grafts.
Aesthetic Zone Management
New approaches for aesthetic zone management including advanced techniques for optimal soft tissue outcomes in visible areas.
Learning Objectives
- Understand the importance of soft tissue management around implants
- Understand the significant differences between periodontal surgeries and implant surgeries regarding soft tissue management
- Be able to choose the ideal autogenous connective tissue graft for soft tissue augmentation around dental implants
- Gain confidence in performing predictable soft tissue augmentation around implants

Prof. Markus B. Hürzeler
DDS, Dr med dent, PhD
About the Instructor
Prof. Markus B. Hürzeler is an internationally recognized expert in periodontics and implant dentistry. He is a specialist in soft tissue management around dental implants and has pioneered numerous surgical techniques that are now considered standard of care in implant therapy.
Prof. Hürzeler maintains a private practice in Munich, Germany, focusing on periodontal plastic surgery and implant dentistry. He is also a visiting professor at multiple universities and has authored numerous peer-reviewed publications on soft tissue augmentation around implants.
His research on the biological width concept around implants and peri-implant soft tissue dimensions has significantly influenced contemporary implant protocols.
Areas of Expertise
- Peri-implant soft tissue management
- Connective tissue grafting techniques
- Aesthetic zone implant surgery
- Free gingival graft modifications
- Periodontal plastic surgery
- Immediate implant placement protocols
Who Should Attend
- Periodontists focusing on implant soft tissue management
- Implant surgeons wanting to improve aesthetic outcomes
- General dentists performing implant surgery
- Clinicians seeking predictable soft tissue augmentation techniques
- Prosthodontists working with implant restorations in aesthetic zones
Workshop Features
- Soft tissue thickness assessment techniques
- Modified free gingival graft procedures
- Connective tissue graft donor site selection
- Aesthetic zone management protocols
- Certificate of completion
Workshop Details

Zygomatic Implants essentials: indications, techniques & Hands-On discovery
Advanced Zygomatic Rehabilitation Techniques
Dr. Sepehr Zarrine
Date
Feb 7, 2026
Time
11:00 - 14:00
Level
Advanced
Fee
S$800
Workshop Overview
This half-day course provides a clear, focused introduction to zygomatic implant rehabilitation. It's suitable for both newcomers and experienced surgeons.
A hands-on workshop reinforces practical insights and essential takeaways for immediate clinical application.
Key Indications
Understanding when zygomatic implants are indicated for atrophic maxillae and severely resorbed cases.
Surgical Principles
Core surgical techniques and decision-making steps for successful zygomatic implant placement.
Hands-On Practice
Practical experience with zygomatic implant techniques on models to reinforce learning.
Learning Objectives
- Understand key indications for zygomatic implants in atrophic maxillae
- Learn core surgical principles and decision-making steps
- Gain hands-on experience with zygomatic implant techniques
- Master prosthetic planning considerations for zygomatic cases

Dr. Sepehr Zarrine
DDS, Oral Surgery Specialist
About the Instructor
Dr. Sepehr Zarrine is an internationally recognized expert in zygomatic implant surgery and complex implant rehabilitation. He has dedicated his career to developing and refining surgical techniques for patients with severely atrophic maxillae who cannot be treated with conventional implants.
With extensive experience in both clinical practice and education, Dr. Zarrine has trained numerous clinicians worldwide in zygomatic implant protocols. He is known for his systematic approach to surgical planning and his commitment to achieving optimal functional and aesthetic outcomes.
Dr. Zarrine has authored multiple publications on zygomatic implant techniques and is a frequent speaker at international implant congresses.
Areas of Expertise
- Zygomatic implant surgery
- Atrophic maxillae rehabilitation
- Full-arch implant solutions
- Complex case management
- Guided implant surgery
- Immediate loading protocols
Who Should Attend
- Oral and maxillofacial surgeons expanding implant options
- Implant surgeons treating severely resorbed maxillae
- Periodontists seeking solutions for complex atrophic cases
- General dentists wanting to understand zygomatic implant referral criteria
- Prosthodontists working on full-arch rehabilitations
Workshop Features
- Indications and contraindications for zygomatic implants
- Surgical techniques and anatomical considerations
- Hands-on practice on simulation models
- Prosthetic planning for zygomatic cases
- Certificate of completion
Workshop Details

Why tongue tie affects growth and airway?
Craniofacial Development
Dr. Irene Lau
Date
Feb 7, 2026
Time
14:00 - 17:00
Level
Intermediate
Fee
S$600
Workshop Overview
The workshop will offer a comprehensive introduction to tongue tie, covering its anatomy, epidemiology, and the most recent research on how it affects feeding, airway function, and oral health.
Anatomy & Impact
- Overview of frenulum structure and its role in tongue movement
- How tongue tie influences feeding, breathing, and oral development
Diagnosis & Assessment
- Identifying key clinical signs and using standardized evaluation tools
- Understanding current debates around diagnostic criteria
Treatment & Follow-up
- Comparing conservative therapies with frenectomy procedures
- Planning risk assessment, postoperative care, and supportive strategies
Learning Objectives
- Understand the anatomical and functional aspects of tongue tie
- Distinguish between types and severity of tongue ties using evidence-based assessment tools
- Develop practical skills in assessment and documentation
- Review current treatment modalities, including indications and contraindications for surgical and non-surgical interventions
- Collaborate in multidisciplinary decision making to deliver patient-centered care
Key Topics Covered

Dr. Irene Lau
Pediatric Dentist & Tongue Tie Specialist
About the Instructor
Dr. Irene Lau is a distinguished pediatric dentist with extensive expertise in diagnosing and managing tongue tie (ankyloglossia) across all age groups. Her clinical practice focuses on the intersection of oral health, feeding difficulties, and airway function, making her uniquely qualified to address the multifaceted nature of tongue tie conditions.
With a commitment to evidence-based practice and multidisciplinary collaboration, Dr. Lau works closely with lactation consultants, speech therapists, myofunctional therapists, and ENT specialists to provide comprehensive care for patients with tongue tie. Her research interests include the impact of ankyloglossia on breastfeeding, speech development, and craniofacial growth.
Areas of Expertise
- Ankyloglossia diagnosis & classification
- Frenectomy procedures
- Infant feeding assessment
- Pediatric oral development
- Airway-focused dentistry
- Multidisciplinary care coordination
Who Should Attend
- Pediatric dentists seeking to expand their tongue tie expertise
- General dentists treating pediatric patients
- Oral surgeons interested in frenectomy procedures
- Healthcare professionals working with infants and children
- Practitioners collaborating with lactation consultants
- Clinicians interested in airway and myofunctional therapy
Workshop Features
- Evidence-based tongue tie assessment protocols
- Standardized classification systems explained
- Treatment decision-making frameworks
- Frenectomy technique overview and considerations
- Multidisciplinary care coordination strategies
- Certificate of attendance
Workshop Details

Advanced flap designs for soft and hard tissue augmentation
Keys for Long-term Implant Stability
Prof. Hom Lay Wang
Date
Feb 8, 2026
Time
08:00 - 11:00
Level
Advanced
Fee
S$1,350
Workshop Overview
This workshop will delve into the critical role of flap design in a variety of periodontal and implant surgical procedures. Participants will engage in in-depth discussions on the key principles behind predictable soft tissue grafting, successful implant placement, and effective bone augmentation.
Tissue Regeneration
- Periodontal guided tissue regeneration
- Predictable bone augmentation procedures
Implant Placement
- Immediate implant placement protocols
- Soft tissue grafting integration
Esthetic Management
- Soft tissue grafting for esthetics
- Managing implant-related challenges
Learning Objectives
- Master step-by-step surgical protocols for periodontal guided tissue regeneration
- Execute immediate implant placement with soft tissue grafting
- Perform predictable bone augmentation procedures
- Apply soft tissue grafting to manage implant-related esthetic challenges
- Incorporate advanced flap designs combining soft and hard tissue augmentation
What's Included
Workshop Details
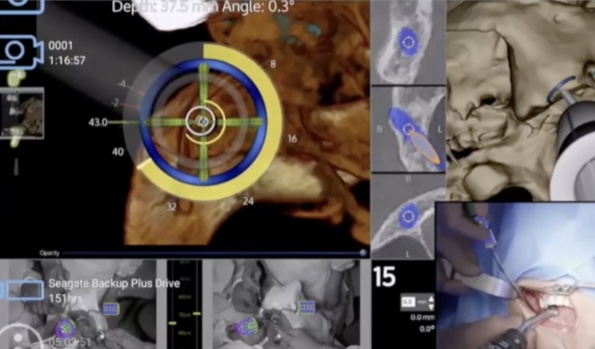
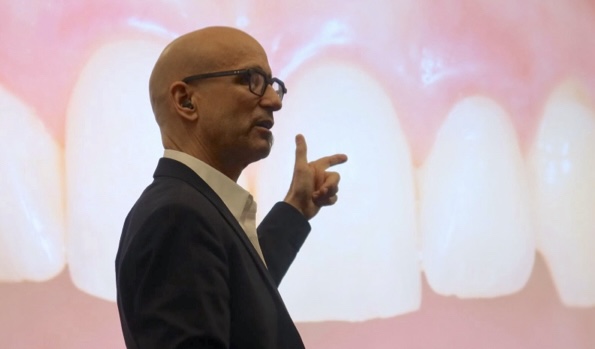
AI-Integrated Full Arch Protocol
Advancements in Navigation, Imaging, Robotic Surgery, and Manufacturing
Prof. James Chow
Date
Feb 8, 2026
Time
11:00 - 14:00
Level
Advanced
Fee
S$600
Workshop Overview
Experience the future of implant dentistry through AI-powered technologies. This hands-on workshop explores cutting-edge navigation systems, advanced imaging techniques, robotic-assisted surgery, and modern manufacturing workflows for full-arch rehabilitation.
Dynamic Navigation
Real-time surgical guidance systems for precise implant placement with live feedback
Robotic Surgery
Robotic-assisted procedures for enhanced precision in complex full-arch cases
Digital Manufacturing
Additive and subtractive workflows for immediate-loading prosthetics
Learning Objectives
- Master the basics of dynamic navigation systems and real-time feedback
- Choose the right imaging method for full-arch implant cases
- Understand the practical role of robotic assistance in complex surgeries
- Compare additive and subtractive workflows for immediate-loading prosthetics
What's Included

Prof. James Chow
BDS, MDS, PhD, FRACDS, FHKAM (Dental Surgery)
Prof. James Chow is a world-renowned pioneer in digital implant dentistry and robotic-assisted surgery. He is the Clinical Director of the Nobel Biocare Innovation Center in Hong Kong and has been at the forefront of integrating artificial intelligence into implant treatment planning and execution.
As a leading researcher in dynamic navigation and computer-guided implant surgery, Prof. Chow has published extensively on the application of AI in dentistry. His groundbreaking work includes developing protocols for robotic implant placement and advancing immediate-loading techniques using digital manufacturing workflows.
Prof. Chow serves as Honorary Professor at the University of Hong Kong and is an active member of the Academy of Osseointegration, ITI, and ICOI. He regularly lectures internationally on digital dentistry and has trained thousands of clinicians in advanced implant techniques.
Who Should Attend
- Oral surgeons seeking to integrate AI technologies
- Implantologists performing full-arch cases
- Prosthodontists involved in digital workflows
- Dental technicians working with CAD/CAM systems
- Clinicians interested in robotic-assisted surgery
Workshop Features
- Live demonstration of navigation systems
- Hands-on experience with AI planning software
- Case studies of robotic implant surgery
- Digital manufacturing workflow demonstrations
- Interactive Q&A with Prof. Chow
Workshop Details

Biomimetic Microstaining Technique
How to simplify daily workflows and create more time for occlusion and function
MDT Edris Rasta
Date
Feb 8, 2026
Time
15:00 - 18:00
Level
All Levels
Fee
S$800
Workshop Overview
Join world-renowned ceramist MDT Edris Rasta for a masterclass in biomimetic microstaining techniques. With over 30 years of experience and lectures in 45+ countries, learn how to create natural-looking restorations while simplifying your daily workflows to focus on what matters most: occlusion and function.
Microstaining Artistry
Master biomimetic staining techniques for lifelike ceramic restorations
Workflow Efficiency
Streamline daily processes to maximize productivity and precision
Occlusion & Function
Focus on functional outcomes for long-lasting aesthetic results
Learning Objectives
- Master biomimetic microstaining techniques for natural tooth aesthetics
- Simplify daily ceramic workflows for increased efficiency
- Understand the relationship between aesthetics and functional occlusion
- Create individualized restorations with patient-centered outcomes
What's Included

MDT Edris Rasta
Master Dental Technician, Laboratory Specialist
MDT Edris Rasta is Chief Ceramist and Owner of Studio Rasta Dental Ceramics Inc., a boutique dental laboratory in Edmonton, Canada. With over 30 years of experience, he is recognized as one of the world's leading ceramists, specializing in natural-looking veneers and full-mouth aesthetic rehabilitation.
A frequent international speaker, Mr. Rasta has lectured in over 45 countries and contributed to major global conferences. He is a published author and collaborates with renowned dentists worldwide, advancing the art and science of dental ceramics.
His philosophy emphasizes precision, individuality, and patient-centered outcomes. His work has set benchmarks in aesthetic dentistry, and his expertise is sought after by dentists who demand the highest standards in ceramic restorations.
Who Should Attend
- Dental technicians seeking advanced ceramic techniques
- Prosthodontists focused on aesthetic restorations
- General dentists interested in ceramic aesthetics
- Laboratory owners looking to enhance workflows
- Ceramists at all experience levels
Workshop Features
- Live microstaining demonstrations
- Hands-on practice with premium materials
- Workflow optimization strategies
- Case studies from MDT Rasta's portfolio
- Interactive Q&A with the master ceramist
Workshop Details

Digital protocol in aesthetic dentistry and micro-preparation (hands-on on phantom heads)
Dr. Marko Jakovac
February 9, 2026
09:00 - 17:00 (Full Day)
M.Vision Center
Limited Seats
S$1800 per participant
Workshop Overview
This workshop will focus on the integration of digital workflows and micro-preparation techniques in aesthetic dentistry. Dr. Marko Jakovac will guide participants through clinically relevant protocols that combine precision, minimal invasiveness, and long-term esthetic success.
Digital Integration
Digital workflow integration for achieving optimal esthetic outcomes with modern protocols
Micro-Preparation
Advanced micro-preparation techniques for minimally invasive aesthetic restorations
Hands-On Practice
Full-day hands-on experience on phantom heads with direct guidance
Learning Objectives
- Understand fundamental principles of digital workflows in aesthetic dentistry
- Identify clinical indications for micro-invasive preparations
- Perform micro-preparation techniques adhering to adhesive dentistry principles
- Evaluate esthetic and functional outcomes of digital restorations
- Communicate effectively with dental laboratory using digital data
- Integrate digital planning with analog skills for optimal outcomes

Dr. Marko Jakovac
Master in Fixed Prosthodontics
About the Instructor
Dr. Marko Jakovac is a renowned expert in digital protocols and oral rehabilitation with extensive expertise in full arch restorations and CAD/CAM technology. He is recognized internationally for his innovative approaches to aesthetic dentistry and minimally invasive techniques.
With decades of clinical experience and academic contributions, Dr. Jakovac has trained thousands of dental professionals worldwide in advanced prosthodontic techniques and digital workflow integration.
Areas of Expertise
- Fixed Prosthodontics
- Digital Dentistry
- CAD/CAM Technology
- Full Arch Rehabilitation
- Oral Rehabilitation
- Digital Workflows
Who Should Attend
- General dentists seeking to enhance aesthetic skills
- Prosthodontists looking to integrate digital workflows
- Restorative dentists interested in micro-preparation techniques
- Dental professionals wanting to improve aesthetic outcomes
- Practitioners interested in CAD/CAM technology
Workshop Features
- Hands-on practice on phantom heads
- Live digital workflow demonstrations
- Direct guidance from Dr. Jakovac
- Comprehensive course materials
- Certificate of completion
Workshop Details

Leveraging 3D printing for provisionalization: from removable to fixed prostheses
Dr. Stephanie Yeung
February 9, 2026
09:00 - 12:00
KLCC Event Center
Limited Seats
S$600 per participant
Workshop Overview
This workshop explores the latest 3D printing technologies and their practical applications in dental provisionalization. Dr. Stephanie Yeung will guide participants through comprehensive digital workflows for creating both removable and fixed prostheses, with emphasis on material selection and clinical optimization.
3D Printing Tech
Understanding 3D printing technologies applicable to dental provisionalization
Removable Prostheses
Workflows for removable prosthesis provisionalization using digital techniques
Fixed Prostheses
Fixed prosthesis provisionalization techniques for optimal patient outcomes
Learning Objectives
- Understand 3D printing technologies applicable to dental provisionalization
- Learn workflows for removable prosthesis provisionalization
- Master fixed prosthesis provisionalization techniques
- Optimize material selection for 3D printed provisionals

Dr. Stephanie Yeung
Digital Prosthodontics Specialist
About the Instructor
Dr. Stephanie Yeung is a leading expert in digital prosthodontics and 3D printing applications in dentistry. With extensive experience in implementing cutting-edge technologies for provisional and definitive restorations, she has become a sought-after speaker and educator in the field.
Her research focuses on optimizing 3D printing workflows for dental applications, with particular emphasis on material science and clinical efficiency. Dr. Yeung has trained numerous dental professionals in adopting digital solutions for their practices.
Areas of Expertise
- 3D Printing Technologies
- Digital Prosthodontics
- CAD/CAM Workflows
- Provisional Restorations
- Material Science
- Digital Dentures
Who Should Attend
- Dentists interested in digital manufacturing
- Prosthodontists seeking 3D printing expertise
- Lab technicians wanting to expand digital skills
- Practitioners implementing digital workflows
- Dental professionals exploring provisionalization
Workshop Features
- 3D printing technology demonstrations
- Material selection guidance
- Digital workflow protocols
- Removable and fixed prosthesis techniques
- Certificate of completion
Workshop Details

Myofunctional Dentistry 101: What Every Dentist Should Know
Understanding Muscle Function in Modern Dentistry
Dr. Donny Mandrawa
Date
Feb 8, 2026
Time
12:00 - 15:00
Level
Advanced
Fee
S$600
Workshop Overview
Unlock the missing link in modern dentistry. This fast-paced, eye-opening workshop shows dental professionals how muscle function drives jaw growth, sleep quality, and treatment outcomes. Learn the patterns you're missing, the red flags you should never ignore, and the tools to transform your approach to patient care.
Muscle-Centric Diagnosis
Develop structured diagnostic protocols outside conventional occlusion models
Airway Integration
Integrate airway and muscle function into growth and retention planning
Sleep-Disordered Breathing
Improve outcomes through myofunctional insight and early intervention
Learning Objectives
- Develop structured, muscle-centric diagnostic protocols
- Integrate airway and muscle function into treatment planning
- Implement early intervention for orofacial dysfunction
- Improve outcomes for sleep-disordered breathing
- Achieve functional harmony between esthetics and muscular function

Dr. Donny Mandrawa
Myofunctional Dentistry Specialist
About the Instructor
Dr. Donny Mandrawa is a pioneering expert in myofunctional dentistry, dedicated to bridging the gap between traditional dental practice and comprehensive muscle function assessment. His innovative approach has transformed how dental professionals understand the relationship between oral muscle function, jaw development, and overall health.
With extensive clinical experience and research in orofacial myology, Dr. Mandrawa has become a leading educator in helping dentists recognize and address myofunctional disorders that impact treatment outcomes and patient quality of life.
Areas of Expertise
- Myofunctional Therapy
- Airway Assessment
- Sleep-Disordered Breathing
- Orofacial Development
- Early Intervention
- Muscle-Centric Diagnosis
Who Should Attend
- General dentists seeking comprehensive patient care
- Orthodontists interested in muscle function
- Pediatric dentists focused on early intervention
- Sleep medicine practitioners
- Dental professionals treating airway disorders
Workshop Features
- Myofunctional assessment protocols
- Airway evaluation techniques
- Sleep disorder recognition
- Patient education materials
- Certificate of completion


